Ongoing Dependent Eligibility Verification
Preserve the integrity of your benefit plan on an ongoing basis by verifying the eligibility of all dependents enrolling in the plan. Conducted after an initial audit or as a stand-alone service, Consova’s ongoing services ensure that only eligible dependents are enrolling in coverage.
Maintain Plan Integrity on an Ongoing Basis
New dependents are added to employer benefit plans for a variety of reasons, including the dependents of new hires, those with qualifying event changes, open enrollment and acquisitions. To ensure that these individuals are eligible at the time of enrollment, employers implement Consova’s ongoing verification services. This can be real-time, weekly, or monthly.
Consova helps organizations conduct ongoing dependent eligibility verification audits to ensure that only eligible dependents are added to benefit plans over the course of a year. On average, roughly 10% of the dependents added mid-year are not eligible for coverage. In addition, it is not uncommon for an employee to attempt to re-enroll an individual that was previously identified as ineligible. Ongoing verifications are the best practice for effectively maintaining the integrity of an employer-sponsored plan.
Sample Savings Scenario
2,134
Dependent Covering Employees
3,690
Dependents Reviewed
$5,000
Average Cost per Dependent
97%
Participation Rate
437
Ineligibles Identified
$1.2M
First Year Savings
When is the Best Time to Verify Newly Added Dependents?

- Directly after Open Enrollment
- Periodic basis throughout POE (Post Open Enrollment)
- In real-time as dependents are enrolled

Experience the Impact of Consova
Recent Clients
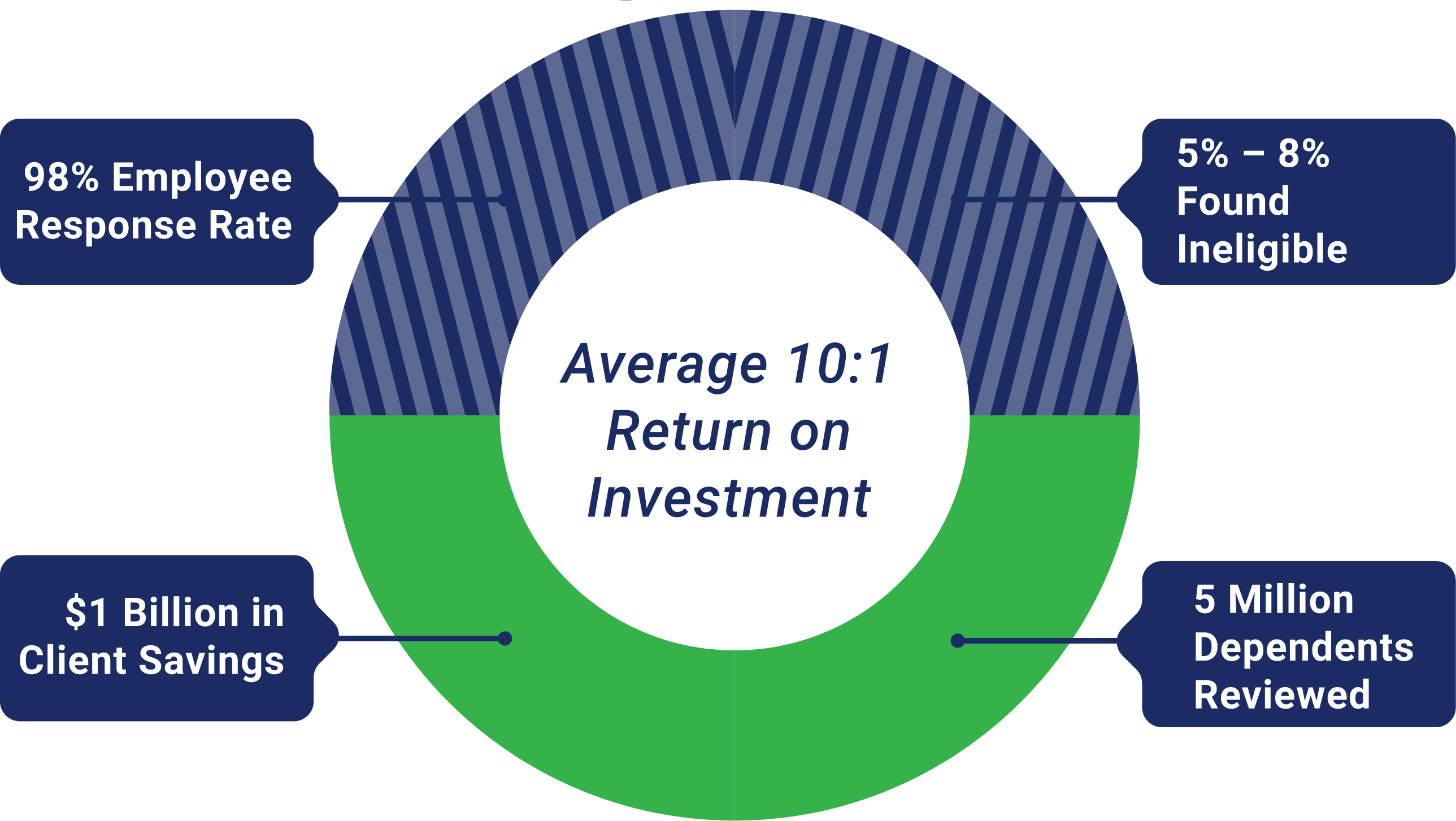
Consova is dedicated to the goal of driving unnecessary costs out of healthcare. Working with household names like Nokia, Sony, Sprint and many others, Consova has delivered over a billion dollars in healthcare savings to our clients.



